By Tim Altman
21/02/2023
Breathing Dynamics, Chronic Illness, Latest News, Naturopathy, Nutrition and Weight Loss, Sleep Enhancement, Testimonials
Breathing, Energy, Fatigue, Memory, obstructive sleep apnoea, Online consultation, sleep apnoea, sleep enhancement, snoring, Tim Altman respiratory theapist
SNORING & OBSTRUCTIVE SLEEP APNOEA SUCCESS CREATES IMPROVED ENERGY, MEMORY & CONCENTRATION & A BETTER RELATIONSHIP WITH PARTNER
Male 64 y.o. complaining of snoring & sleep apnoea.
He’s had a long history of snoring – most of his life. He and his wife sleep in separate rooms as a result.
He complains of feeling fatigued regularly, unrefreshed on waking, experiences frequent headaches, and often has difficulty with memory and concentration.
He was diagnosed with moderate obstructive sleep apnoea several years ago, with 20 apnoea episodes per hour.
He has a CPAP machine, however he hates it and rarely uses it (whilst CPAP technology is considered the gold standard for sleep apnoea treatment, and they definite provide a solution, long term compliance overall is not great, with data varying from anywhere between 15-50% long term compliance).
Other medical information:
High blood pressure – on medication.
Teeth grinding at night – he uses a mandibular advancement device (MAD) via his dentist at night (when not using his CPAP) to reduce this.
Slightly overweight.
Hi average daily diet indicates that he mildly hypoglycaemic, with afternoon slumps in energy, brain fog and desire for refined carbohydrates and sweets. He also relies on coffee to get going each day, and consumes 2-3 coffees per day.
He consumes 2-3 alcoholic drinks 3-4 days per on average, with nothing on the other days.
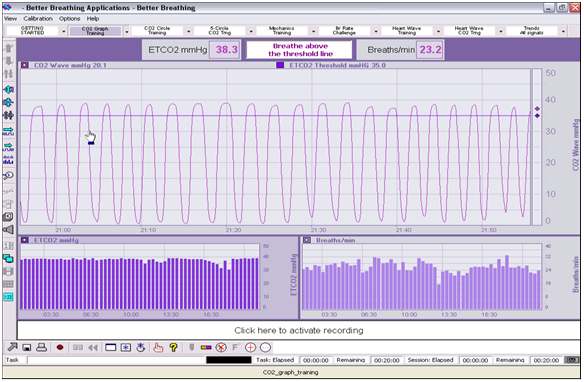
Capnometry biofeedback testing for breathing efficiency revealed that his baseline breathing was between 18-22 breaths per minute (ideally 8-10bpm) with ETCO2 (end tidal CO2 – a measure that is closely correlated to arterial CO2 levels, and indicates breathing efficiency) levels between 28-32mmHg (ideally 40mmHg).
When we slowed his breathing down to 6-8 breath per minute, his ETCO2 levels increases slightly, but not significantly.
However, introducing breathing rhythms where we reduced the volume of breathing significantly, ETCO2 levels raised to between 35-40mmHg. He found the rhythm slightly challenging, but he definitely felt more relaxed, and had more energy.
Therefore the excessive volume of his breathing is a significant contributor to his breathing dysfunction, and one that should be focussed on in treatment.
This client’s objective is to feel more in control of, or eliminate his snoring and sleep apnoea so he can have more energy, mental clarity and overall wellness.
Plus, he’d like to sleep in the same bed with his partner more often, and recreate more intimacy in their relationship. The absence of these in his relationship eats away at him.
Treatment objectives:
Treatment of obstructive sleep apnoea is a multifactorial process that best requires a team of practitioners in specific fields working together. These include dentists & orthodontists, ENT specialists, breathing specialists, nutrition specialists and often musculoskeletal practitioners.
Sleep apnoea is often described in medical terms as sleep disordered breathing, but it is actually the opposite. It is a breathing dysfunction that creates pathological symptoms that severely disrupt sleep. As such, it is breathing disordered sleep.
The chronic symptoms and health problems that follow from snoring and sleep apnoea begin with dysfunctional breathing, and can be fixable by learning how to breathe correctly again.
However, most people, without realising it breathe far too often (twice as often as we should), and with far too much volume because they breathe with their mouth open or with parted lips, rather than with their nose as they should – in other words, we OVER-BREATHE!
And it gets worse at night in bed – particularly as many people sleep with their mouth open.
It is this over-breathing with mouth open that leads to snoring, and the imbalance in the respiratory system that results in apnoea episodes throughout the night, reduced energy production, dry mouth and throat in the morning, and many other symptoms associated with snoring and sleep apnoea.
There are other factors that contribute to and compound snoring and sleep apnoea, and these often need to be addressed also.
However, without addressing over-breathing you’ll always be prone to snoring and sleep apnoea. And many of the issues we mentioned will always bother you.
Addressing the person’s dysfunctional breathing is fundamental to the treatment of snoring and sleep apnoea.
In the case of obstructive sleep apnoea, it is essential to also address the factors that create an obstruction in the person’s airway, as these also contribute significantly to the break down in breathing function in sleep apnoea.
There are several factors that can create obstructions in the airways:
- Obesity – fat gathering in and around the throat.
- Dental Reasons – malpositioned jaw, caused by tension in the muscles.
- Alcohol or drugs relaxing throat muscles.
- Throat weakness – causing it to close during sleep.
- Nasal passage and sinus obstruction.
- Sleeping on the back – leading to the tongue dropping to the back of the mouth.
In mAny cases, lifestyle factors such as obesity, alcohol consumption, sleeping on the back, and stress contribute to a significant amount of breathing obstruction during sleep, and improving these will make the most difference in reducing or removing the obstruction.
Treatment Plan:
- Breathing Dynamics program to retrain breathing to ideal levels – more slowly with less volume, using the nose instead of the mouth. Regular practice of breathing rhythms 2-3 times daily for 10 minutes each time will train the body to breathe more slowly, with less volume habitually on a day to day basis. Similar to geeing fit, the body adjusts to breathing retraining over time. Therefore, this slower, gentler breathing will result in the person being far less likely to snore and over-breathe at night in their sleep, and the resultant imbalance in the respiratory system that results in apnoea episodes in less likely to occur.
- Not sleeping on the back at all – there are some night shirts that have a tennis ball sewn in to the back to prevent sleeping on the back.
- Keeping the mouth closed at night using porous paper tape (i.e. Micropore tape) – mouth breathing is dysfunctional breathing as breathing through the mouth allows up to 6 x the volume of air travelling in and out of the respiratory system, making it far more likely that both snoring, and the resultant imbalance in the respiratory system that lead to apnoea episodes occur.
- As the client hates using his CPAP machine, and rarely (if ever) uses it, we will lead with the above to keep the mouth closed at night. However in the case of some patients who use their CPAP nightly, but would like to reduce their reliance in it over time, we would wean them off this, and onto mouth taping over time, and relying on the CPAP as a back-up if the client has consumed alcohol or is overly stressed etc. I also recommend this client use his CPAP the nights he has consumed excessive alcohol, or was super tired or stressed and taping did not necessarily stick – especially earlier in his practice.
- Reducing alcohol consumption to 2 nights per week only.
- Modifying his diet to regulate blood sugar levels and reduce weight by decreasing consumption of sugar and refined carbohydrates significantly, increasing fruit and vegetable intake, ensuring that at least the first meal of the day has quality protein, having quality snacks comprising nuts & seeds and fresh fruit, and reducing caffeine intake to 1 per day.
- Maintaining use of his mandibular advancement device (MAD) as jaw position can dramatically affect airway openness, and advancing the mandible forward will definitely help to open the airways. Often jaw position is the major, or primary cause of airway obstruction. This is often obvious when the patient is not obese and they do not consume excessive amounts of alcohol, yet they still experience snoring and sleep apnoea.
So this approach to treatment is necessary in most cases.
Outcome:
2 Weeks:
He embraced his program really well, with his breath practice being very consistent and, with the help pf his wife, his nutrition improved dramatically.
Although, he did experience a brief kick back for a couple of days when he reduced his coffee intake, he noticed an improvement in energy and clarity from the nutrition changes fairly quickly. And reducing alcohol intake midweek was not too difficult.
Plus he’s dropped 2kg in weight.
He enjoys the breathing rhythms as he feels calmer and more energised after he does them. He has noticed the rhythms are much easier than when he started, and feels like his breathing is slower and calmer day to day. He’s also noticed that he’s now super conscious of nose breathing all of the time, and picks up both when he, and others are mouth breathing a lot.
His baseline capnometry results at 2 weeks showed that his breathing had slowed to 10-14 bpm on average, and his ETCO2 had improved to 32-35, so some improvements.
He also found it easier to diaphragm breathe, so his capnometry results were much closer to 40 when we simulated the advanced breathing rhythms and fine-tuned his breathing further by continuing to practice breathing with less volume from deeper down (in his pelvic region).
He found it difficult not to sleep on his back initially, but with practice and perseverance, it has become easier, and he rarely finds himself sleeping on his back now.
The mouth taping was initially difficult and he woke during the night and discovered it had come off. However, he retaped and persevered each night.
On a couple of the early nights where the taping did not stick, he used the CPAP to get a decent sleep.
As he started to feel a bit better with his general breathing, and overall wellbeing, he found that he got more used to the mouth taping, and the tape is now staying on more consistently.
He also uses his mandibular advancement device (MAD) more consistently now, and uses it every night he tapes his mouth.
One night on a weekend, he drank too much with friends, and the mouth taping didn’t work too well. So, he surrendered and used his CPAP on this night. He feels like he has a better relationship with his CPAP now – rather than fighting it, it’s there as a back-up on difficult nights where he’s more likely to sleep on his back and/or snore loudly. He estimates he used his CPAP on 30% of nights.
He also sleeps in the same bed as his wife more often now. Approx. half the nights. So he’s happy about that.
His wife has said that his snoring has not gone away, but it has reduced significantly. So she’s also becoming happier.
4 Weeks:
Continued improvements in his nutrition and another 1.5kg reduction in weight.
He continues to enjoy the breathing exercises and notices that he mouth breathes much less, and feels he now breathes primarily using his diaphragm far more often. As such, his breathing rate feels lower, and he feels his breathing and gentler and more calm.
He still has his moments of rapid breathing when he is stressed or he picks up that he is over-breathing at times when he is concentrating.
Sleeping on his side rather than his back has become more habitual, and easier.
Mouth taping has improved and the tape is staying on for the whole night more often.
He is comfortable with using his CPAP as a back-up and used it 20-25% of nights in this 2 week block.
Capnometry testing showed more improvements in baseline breathing rate (10-12bpm) abd ETCO2 35mmHg approx..
Overall he feels like his snoring and apnoea are far more under control, and he knows what he has to do to continue to control it. He really notices the difference if he drinks too much, is stressed or he sleeps on his back.
His wife has reported that she is very pleasantly surprised – he doesn’t snore anywhere near as much, and doesn’t seem to have the pattern of apnoea episodes much at all.
He is wrapped. His initial symptoms of fatigue, waking unrefreshed, poor memory and concentration and regular headaches have improved dramatically.
He has not felt this well for decades, and he feels much more in control of his breathing and his sleep. Plus he loves the reduction in weight, and is starting to exercise more, and feels like he is getting fit.
He loves that he is able to sleep with his partner most nights now, and is very happy that there is more intimacy in their relationship.
Plus he also understands the benefit of his CPAP now, and doesn’t feel like he’s in an ongoing battle with it now – as he did when it was his only option for dealing with his snoring and sleep apnoea.
8 Weeks:
Continued improvements as above in nutrition, breathing on a day to day basis, sleeping position, CPAP when necessary, use of his MAD device, and adherence to mouth taping at night.
He did, however, have a week where they went away on holidays with friends, and his routine went out the door. He consumed far more alcohol and his nutrition was poor.
As such, he noticed big differences in his day to day breathing (if felt more rapid and erratic, coming from the chest and shoulders and mouth more often than his diaphragm and nose).
The mouth taping at night often suffered here as he found himself tending to fall asleep on his back more often, and the tape did not always stay on all night.
He even put on a couple of kgs, so he wasn’t too happy with that.
His wife was also not happy as he snored far more, and his apnoea episodes increased, and there was no option for her to sleep in a spare room, so her sleep suffered also.
He did use his CPAP on a couple of nights, which helped him, but it impacts her sleep.
He felt like he had gone back to square one.
However, on returning to his routine back at home, he was able to bounce back much quicker than expected – within a week. As such, he learned that the changes he had made were rectifiable within a relatively short time by going back to his program and routine.
It also shocked him to see how much lifestyle factors can send his health and symptoms backwards.
The positive from this is that it reinforced the importance of consistent practice of the elements of his treatment program.
It doesn’t require rigid adherence. Just consistent practice. He will have ups and downs, and moments of humanness, however the consistent practice will help him to continue to control his symptoms and his wellbeing, as well being able to feel in control of his sleep quality.
If he continues to improve in his overall health, weight and day to day breathing, plus continuing to use is MAD while sleeping, it is possible over time that he may not need to continue taping his mouth at night. However, he will need to wait until he’s been doing his program for at least 6 months, so that his body can fully adapt and assimilate the changes he’s making.
Then it will be trial and error as to whether he continues taping. Many people continue the process as it guarantees that the mouth will stay closed while sleeping (as long as the tape stays on), and it is not an inconvenience.
Overall, despite the hiccup, this client feels better than he has since he was much younger and very confident that he can continue to be in control of his sleep quality as well as his health and wellbeing all around.
It takes commitment and consistency, however he is very mindful of how unhealthy and out of control he felt prior to beginning this program, so the motivation is strong.
In addition, this improved wellbeing has opened him up to increased exercise and more variety in exercise and lifestyle, so he is super motivated here also.
He is wrapped not only for his improved health & vitality, but also for the improvement in his relationship with his partner.
Moving ahead, I advised him to continue his program as it has been.
Just as it is necessary to maintain good nutrition and quality exercise on a day to day, long term basis, the same applies for breathing and sleep quality practices.
In order to feel the benefits on an ongoing basis, he needs to practice breathing rhythms regularly, continue taping his mouth at night, and using his MAD, as well as using his CPAP machine for back-up at times that his practices slip, or he drinks and eats poorly, or stressed and exhausted.
In addition, it would be ideal for him have regular check-ups with his sleep specialist doctor, his dentist, and his breath specialist.