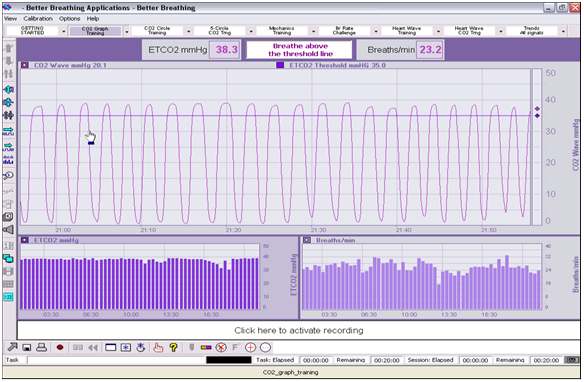
What Capnometry Biofeedback Technology Looks Like and Measures
In a follow up to my last video discussing the potency of Capnometry biofeedback technology for assessing and retraining client’s breathing, I discuss what this technology measures and what you will see on the screen as you are being measured.
Firstly, Capnometry is measuring the volume of carbon dioxide (CO2) in the air that you are exhaling. In hospitals it is used to monitor a patient’s breathing, especially if they are unconscious or have undergone an anaesthetic or are in a coma. The graph starts to curve upwards at the beginning of exhalation (with a slight delay) as CO2 increases, and it curves downwards as exhalation ceases (again, with a slight delay).
The technology provides 2 measurements which give us great information on breathing efficiency for assessment and training:
1. Breathing rate per minute – ideally 8-10 bpm in adults at rest.
2. End-tidal carbon dioxide (ETCO2) – ideally 40mmHg. This is a measurement of the volume of CO2 in the lungs at the end of exhalation. This ETCO2 is essential for respiratory efficiency as it acts as a reservoir of CO2 that permeates back into the blood stream to maintain ideal levels of arterial CO2, which plays a major role in allowing the passage of oxygen from the air we inhale in the lungs, to the cells of the body for energy production. This process is based on the principles of the Bohr Effect and discussed in my last video/post. However, in short, without sufficient arterial CO2 levels. this process is impaired and we produce insufficient amounts of energy, which can lead to fatigue and many other symptoms of illness, including asthma, breathing difficulties, anxiety, sinusitis, snoring & sleep apnoea, headaches & migraines, memory problems, cognitive disturbance etc.
The beauty of this technique is that not only is it fantastic as an assessment of breathing efficiency (non-diagnostic), for breathing retraining it provides in the moment feedback about the efficacy of techniques and rhythms we implement to improve a client’s breathing to ideal, or optimal levels.
As such, we are able to find the best techniques and rhythms specific to each client, and therefore provide them with a specific, individualised breathing retraining program to remove symptoms of illness, improve quality of life and sleep, give them greater energy levels and relaxation, and improve performance.
Breathing as a function, and modality of health is as important and nutrition and exercise. In fact, it is more central than both of these, so it certainly should not be ignored, neglected, or taken for granted (as most of us do).
If you’d like your breathing assessed and to work out an ideal retraining program for your breathing, contact me via me website, www.timaltman.com.au, or email tim@timaltman.com.au.